Geschreven door: Lisette Nijenhuis, aangevuld door Margot van Dijk
Gepubliceerd: april 2025
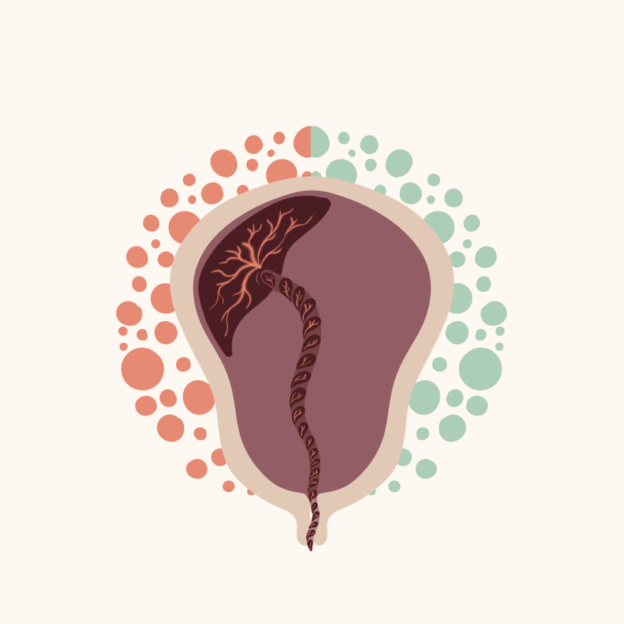
Een vastzittende placenta, ook wel retentio placentae, is een placenta die niet spontaan geboren wordt. Volgens de NVOG is er sprake van retentio placetae als een placenta na dertig minuten niet geboren wordt, of na zestig minuten in een gecontroleerde situatie (waarbij er sprake is van minder dan 500 milliliter bloedverlies, normale controles en een directe operatiekamer voorhanden). Als er sprake is van een retentio placentae moet er worden overgegaan op een manuele placentaverwijdering (NVOG, 2015).
Waarom zit een placenta vast? En waarom zit er een tijdsbestek van dertig of zestig minuten verbonden aan het stellen van de diagnose? Wat als we langer wachten met het stellen van een diagnose? En wat gebeurt er bij een manuele placentaverwijdering? Deze vragen (en meer) worden in dit artikel beantwoord.
Dit artikel gaat specifiek over de vastzittende placenta en de manuele placentaverwijdering na een vaginale baring. Meer informatie over het verloop van het nageboortetijdperk en het beleid dat gevoerd kan worden in deze fase van de bevalling, lees je in het artikel Nageboortetijdperk: afwachten of actief leiden? Meer informatie over een fluxus vind je terug in de masterclass Fluxus in de anamnese – voor zorgverleners of in het webinar Fluxus in de anamnese – voor zwangeren.
- Akol, A. D., & Weeks, A. D. (2016). Retained placenta: will medical treatment ever be possible? Acta Obstetricia Et Gynecologica Scandinavica, 95(5), 501–504. https://doi.org/10.1111/aogs.12848.
- Bais, J., Eskes, M., Pel, M., Bonsel, G., & Bleker, O. (2004). Postpartum haemorrhage in nulliparous women: incidence and risk factors in low and high risk women. A Dutch population-based cohort study on standard (≥500 ml) and severe (≥1000 ml) postpartum haemorrhage. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 115(2), 166–172. https://doi.org/10.1016/s0301-2115(03)00639-0
- Cahill, A. G., Beigi, R., Heine, R. P., Silver, R. M., & Wax, J. R. (2018). Placenta accreta spectrum. American Journal Of Obstetrics And Gynecology, 219(6), B2–B16. https://doi.org/10.1016/j.ajog.2018.09.042
- Cohen, G., Kovo, M., Biron‐Shental, T., Markovitch, O., Daykan, Y., & Schreiber, H. (2023). Risk factors for retained placenta in a first pregnancy—A clinical trial. International Journal of Gynaecology and Obstetrics, 163(1), 194–201. https://doi.org/10.1002/ijgo.14800.
- Combs, C., & Laros, R. (1992). Prolonged third stage of labor: Morbidity and risk factors. International Journal Of Gynecology & Obstetrics, 38(1), 68–69. https://doi.org/10.1016/0020-7292(92)90744-4
- Dehbashi, S., Honarvar, M., & Fardi, F. (2004). Manual removal or spontaneous placental delivery and postcesarean endometritis and bleeding. International Journal of Gynaecology and Obstetrics, 86(1), 12–15. https://doi.org/10.1016/j.ijgo.2003.11.001
- Djaković, I., & Bilić, N. (2014). Acupuncture for retained placenta: A retrospective case series. Acupuncture in Medicine, 32(6), 506–508. https://doi.org/10.1136/acupmed-2014-010607
- Dombrowski, M. P., Bottoms, S. F., Saleh, A. A. A., Hurd, W. W., & Romero, R. (1995). Third stage of labor: Analysis of duration and clinical practice. American Journal Of Obstetrics And Gynecology, 172(4), 1279–1284. https://doi.org/10.1016/0002-9378(95)91493-5
- Edwards, H. M., Svare, J., Wikkelsø, A., Lauenborg, J., & Langhoff‐Roos, J. (2019). The increasing role of a retained placenta in postpartum blood loss: a cohort study. Archives of Gynecology and Obstetrics, 299(3), 733–740. https://doi.org/10.1007/s00404-019-05066-3.
- Endler, M., Cnattingius, S., Granfors, M., & Wikström, A. (2017). The inherited risk of retained placenta: a population based cohort study. BJOG (Oxford. Print), 125(6), 737–744. https://doi.org/10.1111/1471-0528.14828.
- Favilli, A., Tosto, V., Ceccobelli, M., Parazzini, F., Franchi, M., Bini, V., & Gerli, S. (2021). Risk factors for non-adherent retained placenta after vaginal delivery: a systematic review. BMC Pregnancy And Childbirth, 21(1). https://doi.org/10.1186/s12884-021-03721-9
- Fitzpatrick, K. E., Sellers, S., Spark, P., Kurinczuk, J. J., Brocklehurst, P., & Knight, M. (2012). Incidence and Risk Factors for Placenta Accreta/Increta/Percreta in the UK: A National Case-Control Study. PLoS ONE, 7(12), e52893. https://doi.org/10.1371/journal.pone.0052893
- Fujita, K., Ushida, T., Imai, K., Nakano‐Kobayashi, T., Iitani, Y., Matsuo, S., Yoshida, S., Yamashita, M., Kajiyama, H., & Kotani, T. (2021b). Manual removal of the placenta and postpartum hemorrhage: A multicenter retrospective study. Journal of Obstetrics and Gynaecology Research, 47(11), 3867–3874. https://doi.org/10.1111/jog.15004.
- Garmi, G., & Salim, R. (2012). Epidemiology, Etiology, Diagnosis, and Management of Placenta Accreta. Obstetrics And Gynecology International, 2012, 1–7. https://doi.org/10.1155/2012/873929
- Greenbaum, S., Wainstock, T., Dukler, D., Leron, E., & Erez, O. (2017). Underlying mechanisms of retained placenta: Evidence from a population based cohort study. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 216, 12–17. https://doi.org/10.1016/j.ejogrb.2017.06.035.
- Hersh, A. R., Carroli, G., Hofmeyr, G. J., Garg, B., Gülmezoglu, M., Lumbiganon, P., De Mucio, B., Saleem, S., Festin, M., Mittal, S., Rubio-Romero, J. A., Chipato, T., Valencia, C., & Tolosa, J. E. (2024). Third stage of labor: evidence-based practice for prevention of adverse maternal and neonatal outcomes. American Journal of Obstetrics and Gynecology (Print), 230(3), S1046-S1060.e1. https://doi.org/10.1016/j.ajog.2022.11.1298.
- Kamel, A., El-Mazny, A., Salah, E., Ramadan, W., & Hany, A. (2017). Manual removal versus spontaneous delivery of the placenta at cesarean section in developing countries: a randomized controlled trial and review of literature. Journal of Maternal-fetal and Neonatal Medicine/Journal of Maternal-fetal & Neonatal Medicine, 31(24), 3308–3313. https://doi.org/10.1080/14767058.2017.1369522.
- Kristjansdottir, H. L., Bodvarsdottir, S. P., & Sigurjonsdottir, H. A. (2011). Sheehan’s syndrome in modern times: a nationwide retrospective study in Iceland. European journal of endocrinology, 164(3), 349–354. https://doi.org/10.1530/EJE-10-1004
- Kongwattanakul, K., Rojanapithayakorn, N., Laopaiboon, M., & Lumbiganon, P. (2020). Anaesthesia/analgesia for manual removal of retained placenta. Cochrane Library. https://doi.org/10.1002/14651858.cd013013.pub2
- Magann, E. F., Evans, S., Chauhan, S. P., Lanneau, G., Fisk, A. D., & Morrison, J. C. (2005). The Length of the Third Stage of Labor and the Risk of Postpartum Hemorrhage. Obstetrics And Gynecology, 105(2), 290–293. https://doi.org/10.1097/01.aog.0000151993.83276.70
- Manual removal of the placenta | MSF Medical Guidelines. (n.d.). https://medicalguidelines.msf.org/viewport/ONC/english/9-2-manual-removal-of-the-placenta-51417920.html
- Mc, Y., P, L., Wj, S., R, J., J, D., Rr, W., & Cl, H. (2021). Manual Removal versus Spontaneous Delivery of the Placenta at Cesarean Section: A Meta-Analysis of Randomized Controlled Trials. DOAJ (DOAJ: Directory Of Open Access Journals). https://doaj.org/article/6cdf3dd4acc74e4880f08b38642207e3
- NVOG (2015). NVOG-richtlijn Hemorrhagia Postpartum https://www.nvog.nl/wp-content/uploads/2018/02/Hemorrhagia-postpartum-HPP-3.0-14-11-2013.pdf Obstetrische interventies. (2017). In Bohn Stafleu van Loghum eBooks. https://doi.org/10.1007/978-90-368-1744-8.
- Onwuemene, O. A., Green, D., & Keith, L. (2012). Postpartum hemorrhage management in 2012: Predicting the future. International Journal of Gynaecology and Obstetrics, 119(1), 3–5. https://doi.org/10.1016/j.ijgo.2012.07.001 Perined Jaarboek (2017). https://assets.perined.nl/docs/98089ae7-41ae-43ad-800d-5059f81e4c0c.html.
- Perlman, N. C., & Carusi, D. (2019). Retained placenta after vaginal delivery: risk factors and management International Journal of Women’s Health, Volume 11, 527–534. https://doi.org/10.2147/ijwh.s218933.
- Rottenstreich, M., Rotem, R., Bergman, M., Rottenstreich, A., & Grisaru-Granovsky, S. (2019). Recurrence of retained placenta in multiple consecutive deliveries. The Journal Of Maternal-Fetal & Neonatal Medicine, 34(21), 3574–3579. https://doi.org/10.1080/14767058.2019.1688294
- Ruiter, L., Kazemier, B. M., Mol, B. W., & Pajkrt, E. (2019). Incidence and recurrence rate of postpartum hemorrhage and manual removal of the placenta: A longitudinal linked national cohort study in The Netherlands. European Journal Of Obstetrics & Gynecology And Reproductive Biology, 238, 114–119. https://doi.org/10.1016/j.ejogrb.2019.05.022
- Schutte, J. M., Steegers, E. A., Schuitemaker, N. W., Santema, J. G., de Boer, K., Pel, M., Vermeulen, G., Visser, W., van Roosmalen, J., & Netherlands Maternal Mortality Committee (2010). Rise in maternal mortality in the Netherlands. BJOG : an international journal of obstetrics and gynaecology, 117(4), 399–406. https://doi.org/10.1111/j.1471-0528.2009.02382.x
- Say, L., Chou, D., Gemmill, A., Tunçalp, Ö., Moller, A. B., Daniels, J., Gülmezoglu, A. M., Temmerman, M., & Alkema, L. (2014). Global causes of maternal death: a WHO systematic analysis. the Lancet. Global Health/the Lancet. Global Health, 2(6), e323–e333. https://doi.org/10.1016/s2214-109x(14)70227-x
- Shinar, S., Schwartz, A., Maslovitz, S., & Many, A. (2015). How long is safe? Setting the cutoff for uncomplicated third stage length: a Retrospective Case–Control study. Birth, 43(1), 36–41. https://doi.org/10.1111/birt.12200.
- Urner, F., Zimmermann, R., & Krafft, A. (2014). Manual Removal of the Placenta after Vaginal Delivery: An Unsolved Problem in Obstetrics. Journal of Pregnancy, 2014, 1–5. https://doi.org/10.1155/2014/274651.
- VSV Dordrecht (2020) VASTZITTENDE PLACENTA/ MANUELE PLACENTA VERWIJDERING (M.P.V.). https://www.vsvdordrechteo.nl/wp-content/uploads/2021/06/MPV-Vastzittende-placenta.pdf
- Weeks, A. D. (2008). The retained placenta. Best Practice & Research Clinical Obstetrics & Gynaecology, 22(6), 1103–1117. https://doi.org/10.1016/j.bpobgyn.2008.07.005
- WHO (2012). Recommendations for the prevention and treatment of postpartum haemorrhage (2012)https://iris.who.int/bitstream/handle/10665/75411/9789241548502_eng.pdf?sequence=1(2012).
- WHO (2017). Managing Complications in Pregnancy and Childbirth: A guide for midwives and doctors https://iris.who.int/bitstream/handle/10665/255760/9789241565493-eng.pdf
- Zwart, J. J., Richters, J. M., Ory, F., de Vries, J. I., Bloemenkamp, K. W., & van Roosmalen, J. (2008). Severe maternal morbidity during pregnancy, delivery and puerperium in the Netherlands: a nationwide population-based study of 371,000 pregnancies. BJOG : an international journal of obstetrics and gynaecology, 115(7), 842–850. https://doi.org/10.1111/j.1471-0528.2008.01713.x