Gegeven door Margot van Dijk
Gegeven op: 10-09-2024
In deze masterclass neem ik je mee in:
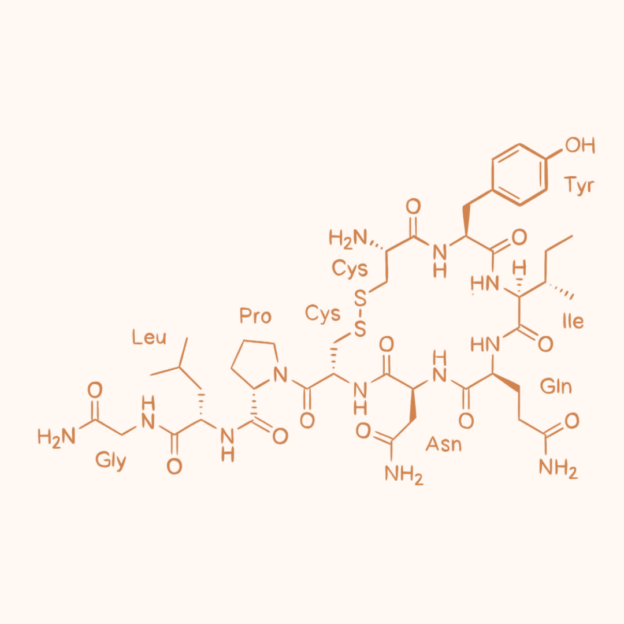
▶️ Hoe oxytocine werkt; als hormoon, neurotransmitter en neuromodulator én wat dat betekent;
▶️ Wat oxytocine receptoren precies doen in het lichaam;
▶️ Welk (levenslang) effect oxytocine heeft op andere hormonen en neurotransmitters bij moeder en kind;
▶️ Wat de impact is van medische interventies op oxytocine;
▶️ Hoe synthetische oxytocine werkt, wat het verschil met lichaamseigen oxytocine en hoe dit tijdens de baring beter kan worden ingezet, met minder nadelige effecten.
Belghiti, J., Kayem, G., Dupont, C., Rudigoz, R. C., Bouvier-Colle, M. H., & Deneux-Tharaux, C. (2011). Oxytocin during labour and risk of severe postpartum haemorrhage: a population-based, cohort-nested case-control study. BMJ open, 1(2), e000514. https://doi.org/10.1136/bmjopen-2011-000514
Bergman N. J. (2014). The neuroscience of birth--and the case for Zero Separation. Curationis, 37(2), e1–e4. https://doi.org/10.4102/curationis.v37i2.1440
Boie, S., Glavind, J., Velu, A. V., Mol, B. W. J., Uldbjerg, N., de Graaf, I., Thornton, J. G., Bor, P., & Bakker, J. J. (2018). Discontinuation of intravenous oxytocin in the active phase of induced labour. The Cochrane database of systematic reviews, 8(8), CD012274. https://doi.org/10.1002/14651858.CD012274.pub2
Buckley, S. J., Childbirth Connection Programs, & National Partnership for Women & Families. (2015). Hormonal Physiology of Childbearing: Evidence and implications for women, babies, and maternity care. Childbirth Connection Programs, National Partnership for Women & Families. https://nationalpartnership.org/wp-content/uploads/2023/02/hormonal-physiology-of-childbearing.pdf
Buckley, S., Uvnäs-Moberg, K., Pajalic, Z., Luegmair, K., Ekström-Bergström, A., Dencker, A., Massarotti, C., Kotlowska, A., Callaway, L., Morano, S., Olza, I., & Magistretti, C. M. (2023). Maternal and newborn plasma oxytocin levels in response to maternal synthetic oxytocin administration during labour, birth and postpartum - a systematic review with implications for the function of the oxytocinergic system. BMC pregnancy and childbirth, 23(1), 137. https://doi.org/10.1186/s12884-022-05221-w
Budden, A., Chen, L. J., & Henry, A. (2014). High-dose versus low-dose oxytocin infusion regimens for induction of labour at term. Cochrane Database of Systematic Reviews, 2016(3). https://doi.org/10.1002/14651858.cd009701.pub2
Dahlen, H. G., Thornton, C., Downe, S., de Jonge, A., Seijmonsbergen-Schermers, A., Tracy, S., Tracy, M., Bisits, A., & Peters, L. (2021). Intrapartum interventions and outcomes for women and children following induction of labour at term in uncomplicated pregnancies: a 16-year population-based linked data study. BMJ Open, 11(6), e047040. https://doi.org/10.1136/bmjopen-2020-047040
Downe, S., & Byrom, S. (2017). Squaring the circle: Researching Normal Birth in a Technological World.
Fewtrell, M. S., Loh, K. L., Blake, A., Ridout, D. A., & Hawdon, J. (2006). Randomised, double blind trial of oxytocin nasal spray in mothers expressing breast milk for preterm infants. Archives of disease in childhood. Fetal and neonatal edition, 91(3), F169–F174. https://doi.org/10.1136/adc.2005.081265
Gholampour, F., Riem, M. M. E., & van den Heuvel, M. I. (2020). Maternal brain in the process of maternal-infant bonding: Review of the literature. Social neuroscience, 15(4), 380–384. https://doi.org/10.1080/17470919.2020.1764093
Hahn-Holbrook, J., Holt-Lunstad, J., Holbrook, C., Coyne, S. M., & Lawson, E. T. (2011). Maternal defense: breast feeding increases aggression by reducing stress. Psychological science, 22(10), 1288–1295. https://doi.org/10.1177/0956797611420729
Insel, T. R. (2010). The Challenge of Translation in Social Neuroscience: A Review of Oxytocin, Vasopressin, and Affiliative Behavior. Neuron, 65(6), 768–779. https://doi.org/10.1016/j.neuron.2010.03.005
Leng, G., Meddle, S. L., & Douglas, A. J. (2008). Oxytocin and the maternal brain. Current opinion in pharmacology, 8(6), 731–734. https://doi.org/10.1016/j.coph.2008.07.001
Pasma, A. (2021). Oxytocine: Knuffelhormoon met Kartelrand.
Peters, L. L., Thornton, C., de Jonge, A., Khashan, A., Tracy, M., Downe, S., Feijen-de Jong, E. I., & Dahlen, H. G. (2018). The effect of medical and operative birth interventions on child health outcomes in the first 28 days and up to 5 years of age: A linked data population-based cohort study. Birth (Berkeley, Calif.), 45(4), 347–357. https://doi.org/10.1111/birt.12348
Selo-Ojeme, D., Rogers, C., Mohanty, A., Zaidi, N., Villar, R., & Shangaris, P. (2010). Is induced labour in the nullipara associated with more maternal and perinatal morbidity? Archives of Gynecology and Obstetrics, 284(2), 337–341. https://doi.org/10.1007/s00404-010-1671-2
Takács, L., Seidlerová, J. M., Štěrbová, Z., Čepický, P., & Havlíček, J. (2019). The effects of intrapartum synthetic oxytocin on maternal postpartum mood: findings from a prospective observational study. Archives of women’s mental health, 22(4), 485–491. https://doi.org/10.1007/s00737-018-0913-3
Thul, T. A., Corwin, E. J., Carlson, N. S., Brennan, P. A., & Young, L. J. (2020). Oxytocin and postpartum depression: A systematic review. Psychoneuroendocrinology, 120, 104793. https://doi.org/10.1016/j.psyneuen.2020.104793
Uvnas-Moberg, K. (2003). The oxytocin factor: tapping the hormone of calm, love, and healing. https://openlibrary.org/books/OL3676350M/The_oxytocin_factor
Uvnas-Moberg, K. (2016). Oxytocin: The Biological Guide to Motherhood.
Walter, M. H., Abele, H., & Plappert, C. F. (2021). The Role of Oxytocin and the Effect of Stress During Childbirth: Neurobiological Basics and Implications for Mother and Child. Frontiers in endocrinology, 12, 742236. https://doi.org/10.3389/fendo.2021.742236
Lopend onderzoek naar discontinueren van synto: https://onderzoekmetmensen.nl/en/node/47801/pdf